Reimbursements
Certain payors will reimburse for tele-health services equal to office
visits while others may not or have certain requirements.
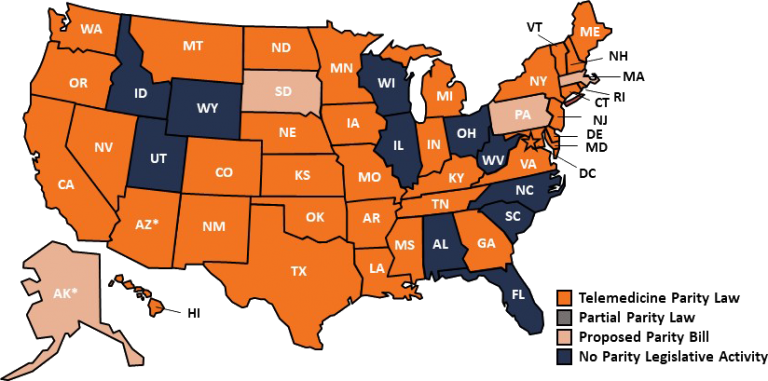
Currently, there are 33 states that have parity laws that mandate
private payer reimbursement for telemedicine services. To learn more,
visit the
American Telemedicine Association
You may also visit the
Center for Connected Health Policy
to learn more about patient and provider requirements that determine
reimbursement. Additionally, they provide in-depth information on
legislation for both public and private healthcare programs and is a
fantastic resource for those looking to dive deep into individual
state policy.
Private Pay
Parity laws allow for providers to be paid at the same rate
irrespective of whether services are provided by telehealth or
in-person. Parity laws are equalizing payments with traditional
practice. Each provider must review their private payor contracts to
determine what services are eligible for telehealth.
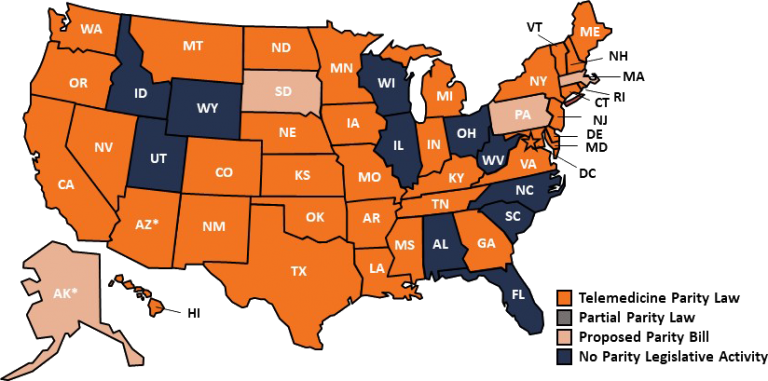
Footnote: A map of state parity law status around the country.
Medicare
Medicare currently pays for telehealth services, but with a major
asterisk. They are required to be provided only in rural or in
provider shortage areas and must be provided at certain types of
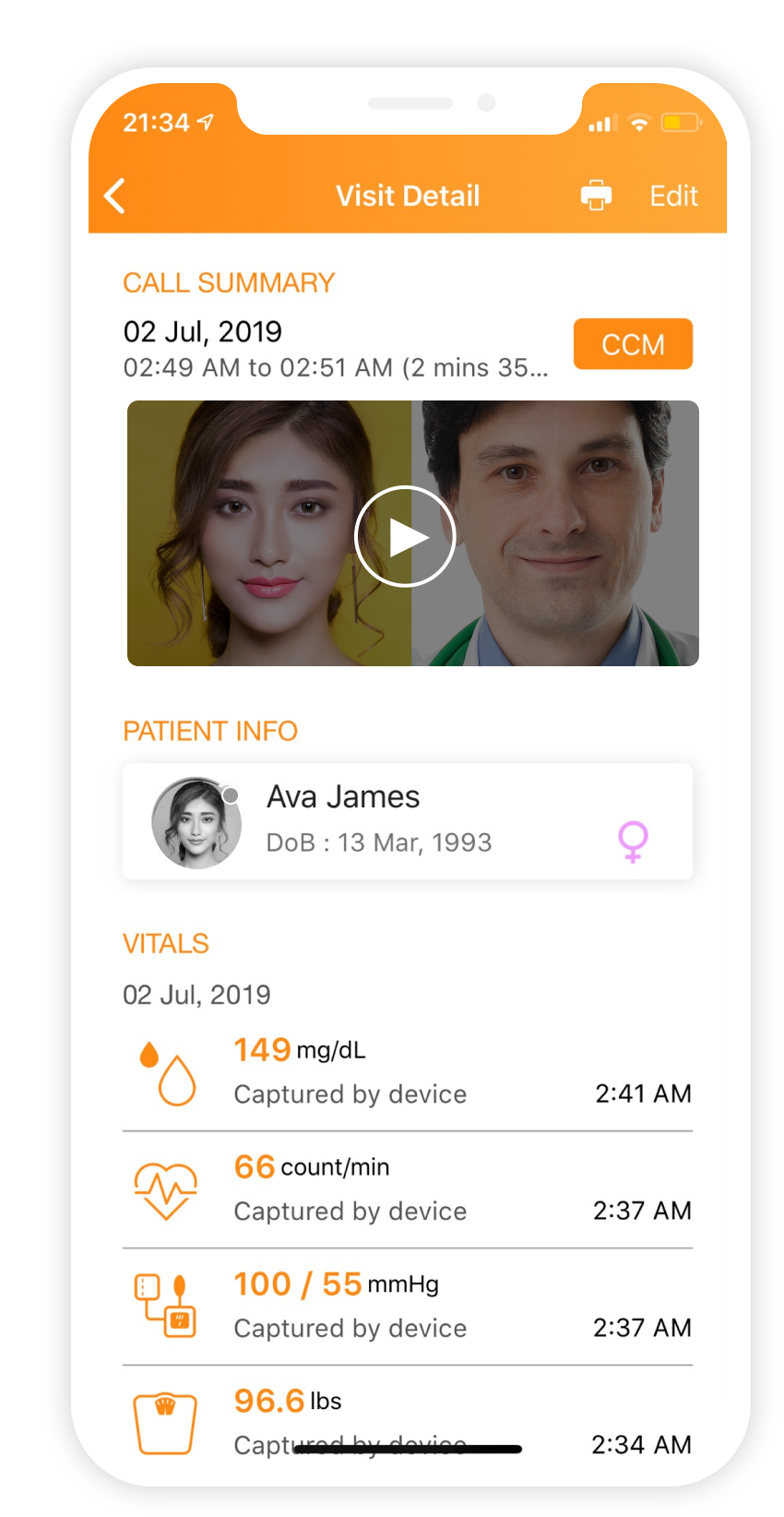
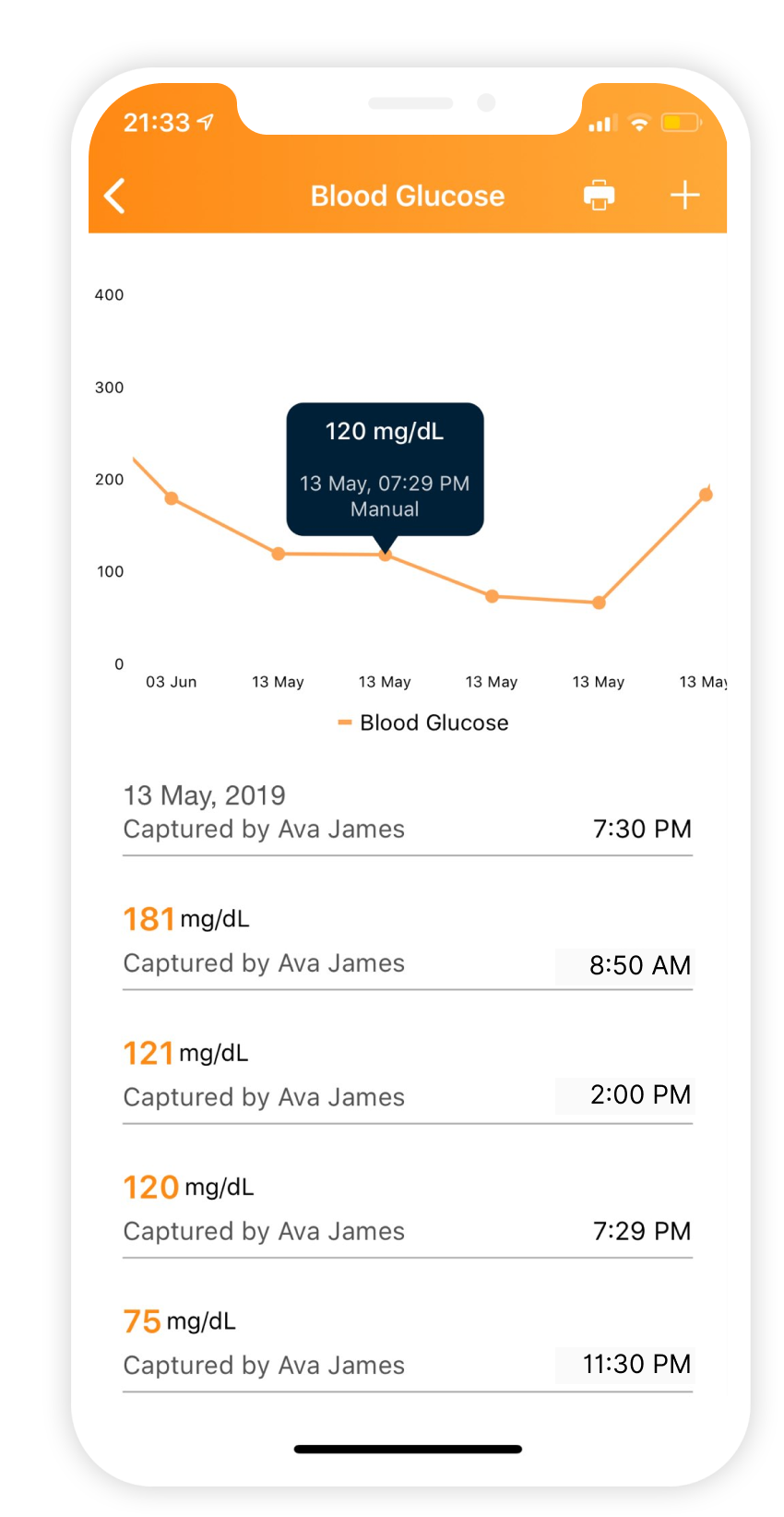
facilities. Medicare does allow telehealth services for CCM (chronic
care management) and RPM (remote patient monitoring) to be paid for
regardless of patient or provider location. And now they are also
allowing demonstration projects for ESRD (end stage renal disease)
patients to provide telehealth services irrespective of their location
Medicaid
Medicaid allows for all tele-health services in 49 states. Refer to
the
CCHP
website for state-specific details
Capitated Pay
Telehealth is a very useful tool to decrease cost of care for
capitated providers while still providing significant improvement for
access to care of patients.
Self Pay
Direct pay providers may charge patients their own custom rates for
concierge care.